RP is a 68 year-old male who was admitted to the hospital from his long-term care facility after 1 week of dyspnea and cough
RP is a 68 year-old male who was admitted to the hospital from his long-term care facility after 1 week of dyspnea and cough
RP is a 68 year-old male who was admitted to the hospital from his long-term care facility after 1 week of dyspnea and cough. He was seen by a staff physician at the long-term care facility and was diagnosed with a COPD exacerbation. He was prescribed azithromycin, but has not improved after 3 days of antibiotics. He has a history of dyslipidemia, COPD, alcoholic cirrhosis, and HTN. He routinely takes lisinopril, atorvastatin, tiotropium and fluticasone/salmeterol, and has recently had a heavier reliance on his rescue albuterol inhaler.
Vital signs:BP: 140/86, HR: 89, RR: 18, TMAX: 102.2°F, O2 saturation: 84% on 4LNC, Pain 0/10
Assessment findings: alertness slightly altered, but baseline, coarse breath sounds, rhonchi and wheezesheard throughout with an occasional productive cough, dyspnea is worse than baseline; regular rate and rhythm, no murmurs, no edema, decreased peripheral pulses bilaterally, feet cool to touch; abd slightly distended; skin excoriated, otherwise normal
Requirements: 2 pages
ORDER NOW FOR CUSTOMIZED, PLAGIARISM-FREE PAPERS
Assignment # 3 Mini Concept Map
Using this scenario:
RP is a 68 year-old male who was admitted to the hospital from his long-term care facility after 1 week of dyspnea and cough. He was seen by a staff physician at the long-term care facility and was diagnosed with a COPD exacerbation. He was prescribed azithromycin, but has not improved after 3 days of antibiotics. He has a history of dyslipidemia, COPD, alcoholic cirrhosis, and HTN. He routinely takes lisinopril, atorvastatin, tiotropium and fluticasone/salmeterol, and has recently had a heavier reliance on his rescue albuterol inhaler.
Vital signs:BP: 140/86, HR: 89, RR: 18, TMAX: 102.2°F, O2 saturation: 84% on 4LNC, Pain 0/10
Assessment findings: alertness slightly altered, but baseline, coarse breath sounds, rhonchi and wheezesheard throughout with an occasional productive cough, dyspnea is worse than baseline; regular rate and rhythm, no murmurs, no edema, decreased peripheral pulses bilaterally, feet cool to touch; abd slightly distended; skin excoriated, otherwise normal
Discharge Plan:
LabsMicro
Na: 141Creatinine: 1.6Blood Culture: No growth at 48 hrs
K: 4.2WBC: 19.6Gram Stain: 4+ squamous, no organisms
Cl: 98Hgb: 10.8Culture: No growth at 48 hours
Bicarb: 23 Hct: 36.2Pneumococcal:Positive
BUN: 24 Platelets: 300
Radiology Chest X-ray showed focal consolidation in the right lower lobe, suggestive of pneumonia.
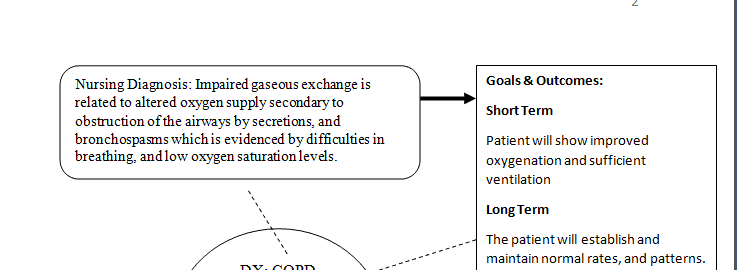
You are expected to develop 2 actual nursing diagnosis for your patient. Only use 1 Nursing Diagnosis per page
Assign 2 priority interventions for EACH Nursing Diagnosis
Establish 1 short term goal
Establish 1 long term goal
For the short-term goal, was your patient able to meet it? If so, how was that demonstrated. If not, what could you do differently to help the patient to meet the goal?
Please use the sample concept map below for the 2 Nursing Diagnosis you selected